The phrase “just in the nick of time” can be traced back to 16th century England when the word “nick” meant “the critical moment.”
For Jeff Cowan, a 63-year-old medical transport driver, that phrase also describes the care he received at Oklahoma Heart Institute (OHI) that saved his life.
The Tulsa resident was visiting his doctor after hip replacement surgery at another Oklahoma hospital. Cowan asked the doctor about his leg, which was swollen below the knee. The doctor asked how long he had been wearing compression socks and suggested he begin wearing loose-fitting socks again.
“A few weeks later during the summer heatwave, I was helping my wife Liana carry in some groceries when I collapsed,” Cowan recalled. “I remember thinking, ‘this must be heatstroke,’ so I got up and went inside to lie down and get cool.”
After a short time, Cowan was still feeling faint. “I just couldn’t get it back together mentally or physically after falling,” he said. “I was communicating fine and everything, but just barely making it. That’s when we decided that I needed to go to the hospital.”
Cowan’s wife drove him to the Emergency Department at Hillcrest Medical Center. The triage staff told Cowan they were glad he came in, as it looked like he had a blood clot in his leg.
After the examination, the ER staff was concerned that they may have to operate on the leg, perhaps amputating it. Within a few hours, however, they determined that the blood clot had moved up Cowan’s leg and was now lodged in his lungs, becoming a pulmonary embolism.
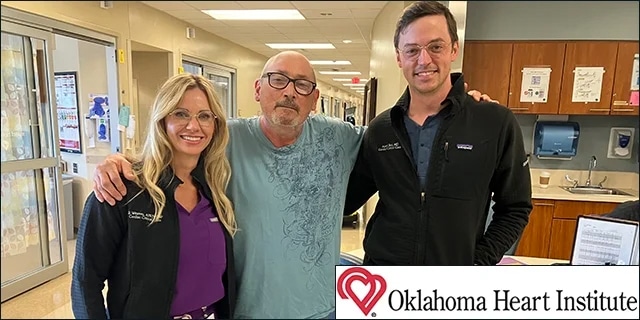
Cowan was rushed to Oklahoma Heart Institute where he was placed under the care of Adam Betz, M.D., and Brooke Weaver, APRN-CNP (both shown in the above photo on either side of Jeff Cowan). Dr. Betz is the Medical Director of Cardiovascular Critical Care and Medical Director of ECMO.
ECMO at work
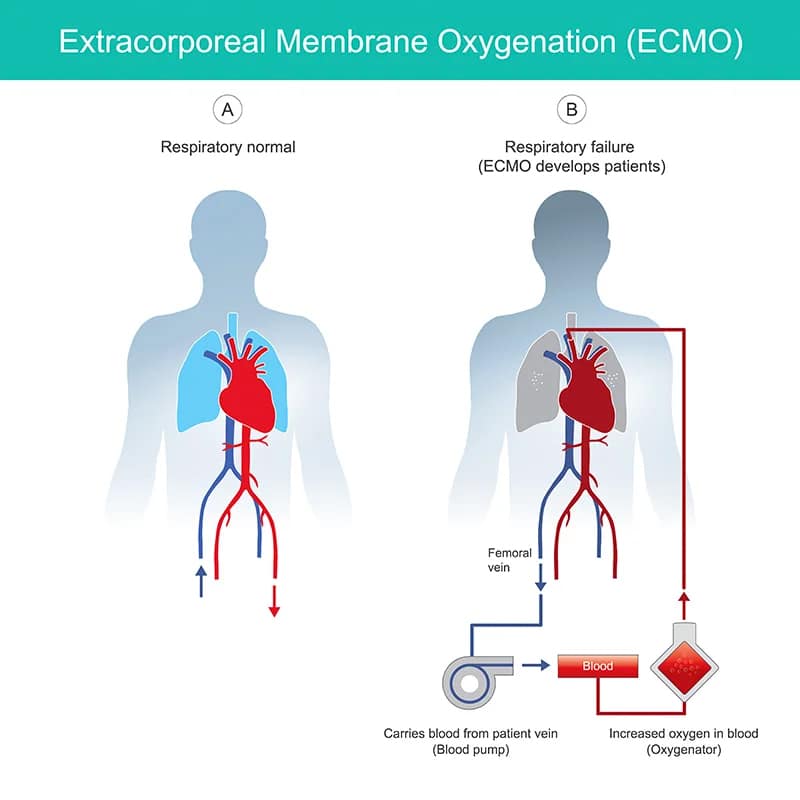
“When Mr. Cowan arrived at OHI, his cardiac vital signs started to crash, so we rushed him to the cardiac cath lab,” recalled Dr. Betz. “At my request, Kamran I. Muhammad, M.D. put Cowan on ECMO.
“ECMO, which stands for Extracorporeal Membrane Oxygenation, is a machine that functions as either an artificial heart or artificial lung, allowing patients to rest their heart and lungs while their blood is being re-oxygenated.
“In Mr. Cowan’s case, it kept him stable while another doctor operated to remove the clot in his lungs,” said Dr. Betz.
According to his wife Liana, after his successful surgery, Cowan remained in the cardiac intensive care unit for 30 days and then spent about a week in another room on the floor.
Watch a video about ECMO
Rehabilitation at the park
As soon as he was able, staff members got Cowan up on his feet to walk short distances and begin his rehabilitation from surgery. “It was a little tough at first since I was sore, but they got me up and moving around,” Cowan said.
Once discharged from the hospital, Cowan returned home and remained active by working part-time and taking walks with Liana.
“We like going down to Braden Park and feeding the ducks – basic old people stuff,” he joked. “We’ve been married 38 years and enjoy spending time together. We love to cook and eat good food at home. Two of our favorite meals are salmon with asparagus and Jack Daniel’s Barbecue with a small macaroni salad.”
He is also grateful for the excellent care he received at Oklahoma Heart Institute.
“I credit the ECMO for being the factor that put me over the hurdle between life and death,” he said. “But if it wasn’t for Dr. Betz and his staff, I don’t know what would have happened. They are the gold standard of medical staff, as far as I’m concerned.”
Cowan also praised Dr. Betz for being aggressive with his condition.
“He is not afraid to go after a problem,” said Cowan. “A pulmonary embolism is a silent killer. You may not even know if you have one until too late. Thankfully, Dr. Betz didn’t stand back and think too long about what I needed. If he had, I would be dead. I think he’s a fabulous doctor and the staff at OHI are all fantastic.”
Click here to read more about Oklahoma Heart Institute’s cardiovascular critical care unit and our ECMO equipment. For ECMO referrals, please call 1-833-OHI-ECMO (644-3266).