Our Electrophysiology Team strives to provide state-of-the art arrhythmia care to patients within and outside our community. Our nationally-recognized EP team’s approach can be witnessed both in the hospital and in the office.
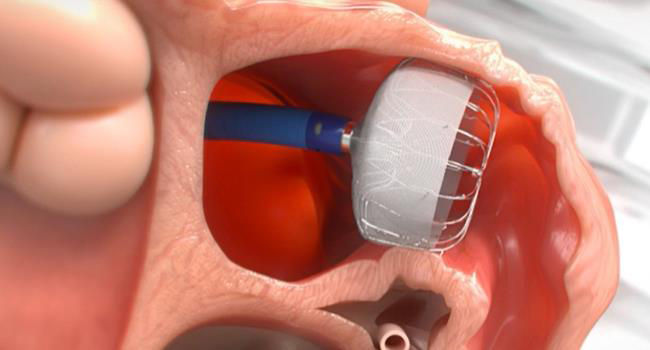
There is no field within cardiology that has undergone as much change in the last decade than the field of electrophysiology (EP). With advances in catheter-based ablation and implantable cardiac devices, we are able to tackle (and frequently cure) diseases previously considered untreatable.
We do this in many ways. First, we keep up with national trends and the newest procedures. The board-certified physicians and staff of Oklahoma Heart Institute attend national and regional meetings to make sure we are at the cutting edge of arrhythmia management. This allows us to perform not only simple ablation such as supraventricular tachycardia (SVT) and atrial flutter, but also complex ablations including atrial fibrillation and ventricular tachycardia.
Second, we educate our local community so that they can help us identify and treat patients in the most appropriate way. Our annual EP Symposium attracts over 300 healthcare providers from throughout the region. We also host quarterly Tulsa EP Society (TEPS) meetings which are aimed at local physicians, physicians-in-training and staffs of all Tulsa’s EP community.
Third, we participate in numerous research studies. This allows our patients to access medications and devices prior to market release. Examples of research studies we offered our patients include the ATHENA Trial and the Re-Ly Trial. These trials (both published in the New England Journal of Medicine) showcased dronedarone and dabigatran – medications which will change the way we treat atrial fibrillation for years to come.
Last, we collaborate extensively with our non-EP colleagues. We understand that patients often have complex medical issues that require thoughtful discussion with a variety of specialists. Because Oklahoma Heart Institute includes many subspecialists, including cardiovascular surgeons, interventional cardiologists and heart failure specialists, we are able to join forces to streamline your care like no one else.
If you or a loved one needs to see an arrhythmia specialist, the EP Team at Oklahoma Heart Institute will provide you with the best care available. We look forward to earning your trust and having you see what sets us apart.
Heart Rhythm Service
Oklahoma Heart Institute’s Heart Rhythm Service is the largest team of electrophysiology specialists in northeast Oklahoma offering state-of-the-art arrhythmia care. They provide a full array of advanced services to patients who need help regulating their heart rhythm including evaluation, diagnosis and therapy for conditions such as atrial fibrillation, ventricular arrhythmias and devices for congestive heart failure.
Our electrophysiology team specializes in catheter ablation for a variety of heart rhythm abnormalities. Also, every year they implant hundreds of pacemakers and defibrillators with cutting edge techniques to maintain or resynchronize the heart’s normal conduction system. Each device is carefully chosen to ensure its specific features are tailored to their patient’s needs. Our Heart Rhythm Service also provides the regular monitoring and adjustments needed to ensure all devices are performing effectively. Thousands of pacemaker evaluations are performed yearly by their electrophysiologists and specialized pacing nurses.
Contact Us
For more information or to schedule an appointment, please call 918-592-0999.
Heart Rhythm Service Providers
Click on a Provider to View More Information