The Advanced Heart Failure Center
The Advanced Heart Failure Center at Oklahoma Heart Institute (OHI) is a recognized Get With The Guidelines® Heart Failure center that provides comprehensive cardiac care to patients with advanced heart failure and pulmonary hypertension. We specialize in the evaluation and implementation of treatment plans for patients with complex cardiovascular disease with the goal of cardiac recovery. In those patients who experience progression of disease and are eligible, we provide an array of advanced therapies including continuous home infusions, implantation of durable left ventricular assist devices (LVADs), timely referral to a transplant center and access to greater support at home in the form of palliative or hospice care.
Our center utilizes a comprehensive multidisciplinary approach for the care of our patients. We work closely with various medical and surgical specialties and subspecialties available at OHI to manage our patients. We are a key step in the evaluation and referral process to a variety of FDA-approved percutaneous valvular replacement interventions performed by our highly trained structural cardiology team (TAVR, Mitra-clip, Mitral II trial, CLASP IIF trial, TRISCEND II trial). We have also expanded the therapeutic armamentarium available to advanced heart failure patients to include devices that seek to improve patient’s symptoms, like the Barostim device, or treat a once untreatable condition in patients with reduced ejection fraction, such as central sleep apnea with the remedē® System.
We are the only center in Tulsa supported by an extracorporeal membrane oxygenation (ECMO) program, which allows us to support and bridge many of our patients safely to recovery or to the implantation of a durable heart pump (left ventricular assist device) or heart transplant. Our team of highly trained cardiologists, intensivists, surgeons, advanced practice providers, specialized nurses, cardiac care coordinators, social workers, case managers, therapists, exercise physiologists and other experts are at the disposition of our patients to improve their symptoms, quality of life and survival.
For patients
The patient is our top priority at the Advanced Heart Failure Center. We will provide the education and tools needed to understand the diagnosis of heart failure or pulmonary hypertension, and the treatment options available to you.
What to expect at the first appointment:
We ask that you arrive 15 minutes early to fill out the necessary paperwork and to bring all medication bottles with you. After meeting with the provider, one of our nurses will meet with you to provide heart failure education. We also provide you with a blood pressure cuff, weight scale and water bottle to help with the daily management of your heart condition.
What to expect at each appointment:
Please bring your medication bottles and daily weight/blood pressure log with you to every appointment. Each time, we will take your weight and vital signs.
Our clinic has a nurse on-call 24/7 for emergencies. Our goal is to manage your care outpatient and keep you out of the hospital.
For providers
Our team of physicians, advanced providers and nurses specialize in the diagnosis and treatment of advanced heart failure and pulmonary hypertension. The clinic is located within the OHI hospital, on the campus of Hillcrest Medical Center, which allows us to provide a comprehensive fluid management program, including evaluation and treatment with intravenous diuresis, hydration and electrolyte replacement in the outpatient setting. We can obtain electrocardiograms, telemetry monitoring and collection of labs with same-day results. Rapid assessment of the efficacy of outpatient therapies facilitates the decision to discharge home versus direct-admit to the hospital for further escalation of care. The clinic has a nurse on-call 24/7 for emergencies. Our highly specialized registered nurses provide every new patient consult with heart failure education and continued re-enforcement. Our goal is to reduce hospital readmissions and improve patients’ quality of life.
Please keep in mind an early referral is essential in those patients whom we suspect are progressing into advanced heart failure and require an evaluation for advanced therapies, including transplant or LVAD evaluation. We believe in a shared care model within our practice and encourage patients to continue their follow-up visits with those referring physicians who would like to remain involved in the management of their patients’ care.
Please see below for the wide range of services we provide here in the Advanced Heart Failure Center. We look forward to partnering with you.
ALT-FLOW II Clinical Trial
Contact Us
For more information about The Advanced Heart Failure Center, please call 918-574-9003.
Referral Information
For urgent inpatient referrals, please call 1-833-OHI-ECMO (644-3266)
For non-urgent outpatient referrals, please call 1-833-OHI-LVAD (644-5823)


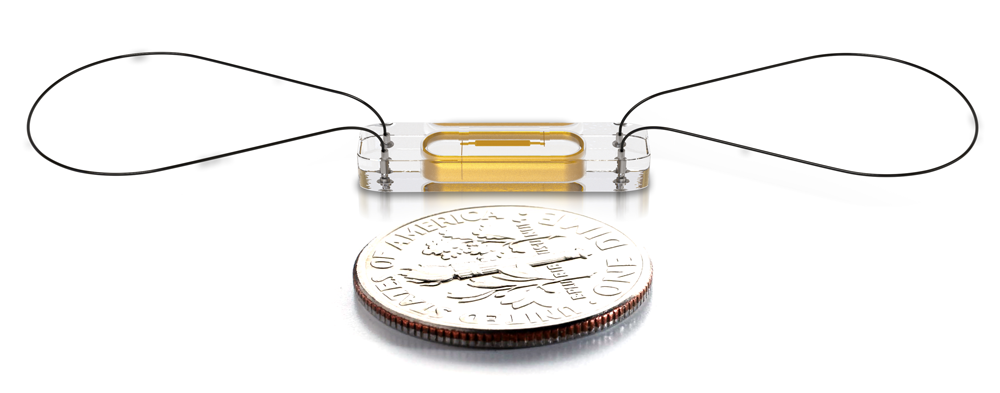 Photo courtesy of Abbott
Photo courtesy of Abbott