Atrial fibrillation (AFib) is frequently characterized by a fluttering sensation in the chest. It is a type of irregular, often rapid heartbeat resulting from the atria beating out of sync with the ventricles. While AFib itself isn't immediately life-threatening, it can elevate your risk of developing blood clots and stroke.

David Sandler, M.D. is an electrophysiologist at Oklahoma Heart Institute (OHI). He shares risk factors for AFib, what issues the irregular beat can cause and how to avoid AFib. Mike Roberson, a patient with OHI, reflects on his experience with AFib and how he’s recovering from a stroke caused by a blood clot that developed while he had AFib.
What is AFib?
“Atrial fibrillation is the most common sustained abnormal heart rhythm,” said Dr. Sandler. “Normally, the top chamber of the heart, the atrium, squeezes the blood at about 60 beats per minute. When in atrial fibrillation, instead of squeezing blood, the atrium just quivers.”
Sustained atrial fibrillation can cause blood in the atrium to reach stasis, which makes it pool and thicken. Blood clots can form, which can travel to the brain and lead to strokes. Managing AFib is not just controlling its symptoms, but also managing risk factors for other potential complications like stroke, which makes it different from other heart rhythm abnormalities.
Symptoms of AFib
While some people describe AFib as having butterflies or even a flopping fish in their chest, others experience chest pain, dizziness, shortness of breath and fatigue. For some, AFib symptoms may continue for hours, days, weeks, months or even years.
“The most classic symptom of Afib is the heart beating rapidly and irregularly,” said Dr. Sandler. “Patients have told me that it feels like squirrels wrestling in their chest, Morse code in their chest. What's now becoming more common is the detection of AFib during routine testing after they have no symptoms.”
This is what happened to 73-year-old Mike Roberson. In 2013, the Tulsa native was diagnosed with atrial fibrillation while undergoing a pre-op electrocardiogram (EKG) before gallbladder surgery.
“My heart doesn’t race, I have a very low heart rate, so my AFib was kind of weird,” said Roberson. “I never had any shortness of breath or rapid heart rate. I’m very healthy, I haven’t caught a cold in years, and I go to the gym two or three times a week.”
Roberson’s gallbladder surgery was suspended until he could be seen by a cardiologist. He saw OHI cardiologist Frank Gaffney, M.D., who told him that he should start taking blood thinners to lower his risk of blood clots and stroke.
“I thought my AFib was very mild, and I told him I never had any bad experiences,” said Roberson. “Dr. Gaffney told me my first unpleasant experience with AFib may be a stroke. But I didn’t really want to go on blood thinners. I didn’t think I had a serious problem, so I didn’t take them.”
AFib complications
Roberson’s atrial fibrillation contributed to a blood clot that caused a stroke on May 24, 2023. He went to the restroom that morning, and his wife Shirley noticed him taking a long time. When she checked on him, he was leaning against a wall and answering her questions with strange phrases.
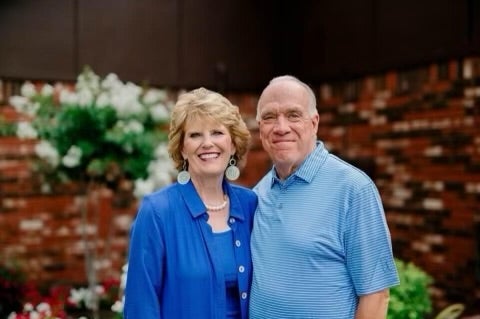
“He had no slurred speech or anything,” said Shirley Roberson. “I told him to raise both arms, and he only raised his right arm. That’s when I knew he was having a stroke.”
His wife called 911 and Roberson was taken immediately to Hillcrest Medical Center. When someone experiences a stroke, there is a very small window of time to get them the critical care they need to prevent severe brain damage or death. Doctors quickly gave Roberson clot-busting medicine and performed a thrombectomy to remove the blood clot. Roberson’s stroke was classified as moderate to severe.
“I don’t remember the EMTs or the ambulance,” said Roberson. “I don’t remember anything until I was in the ICU.”
After 36 hours, Roberson was transferred from the ICU to inpatient rehabilitation. He had to re-learn how to walk, talk and eat over the course of nearly two weeks. He was released from outpatient rehab in August 2023 and was back to his normal life just three months after his stroke.
“After this experience, I 100% agree that you need to listen to your physician if you have any heart issues at all,” said Roberson. “If they say you need a blood thinner, I recommend that you listen to them and take it. Anything that you can do to reduce the chance of stroke, you should do it.”
“He probably wouldn’t have had a stroke at all if he had been on blood thinners,” said Shirley Roberson. “He had a happy ending to his story, but most people don’t.”
Risk factors
Many conditions can increase your risk of atrial fibrillation, including:
- Age
- Nicotine or alcohol use
- Obesity
- Sleep apnea
- Family history
- High blood pressure
Atrial fibrillation can be managed by also controlling these risk factors. Dr. Sandler said losing weight and reducing alcohol consumption are the two best ways to prevent or manage AFib.
"There are therapies out there to help. To treat AFib, we have to decide which part of the condition we’re going after,” said Dr. Sandler. “I tell patients there are two buckets: one that can help protect them from stroke, including pills and procedures. The second bucket is things we can do to make them feel better, which include pills, ablation procedures and pacemakers.”
Oklahoma Heart Institute offers a variety of these treatment options for atrial fibrillation. Dr. Sandler welcomes new patients at OHI on the campus of Hillcrest Medical Center, Hillcrest Claremore and OHI’s South Pointe office at 92nd and Mingo in Tulsa. To make an appointment and speak to a doctor about your Afib treatment options, visit this link or call 918-592-0999.

